登录方式
方式一:
PC端网页:www.rccrc.cn
输入账号密码登录,可将此网址收藏并保存密码方便下次登录
方式二:
手机端网页:www.rccrc.cn
输入账号密码登录,可将此网址添加至手机桌面并保存密码方便下次登录
方式三:
【重症肺言】微信公众号
输入账号密码登录
注:账号具有唯一性,即同一个账号不能在两个地方同时登录。
作者:徐海博
单位:河北医科大学第二医院呼吸与危重症医学一科
# 一、插管设计 #
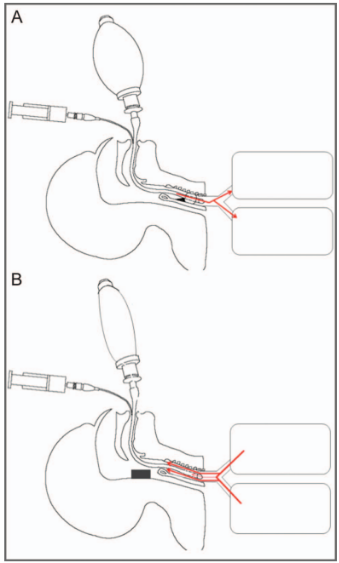
图源:Respir Care. 2017 Aug; 62(8):1007-1013.
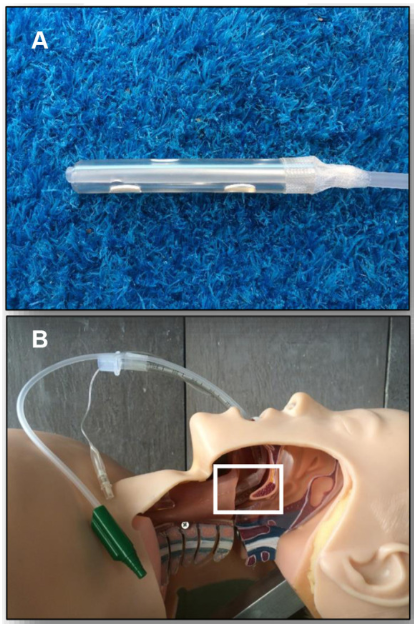
图源:Med Devices (Auckl), 2021, 14:287-297.

# 二、气道管理 #
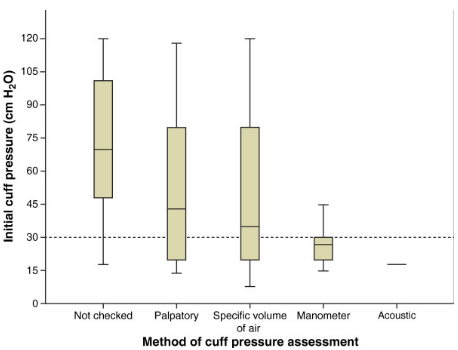
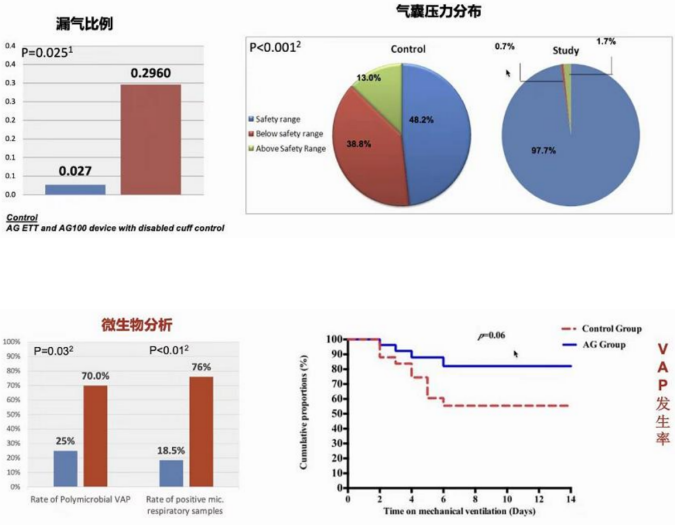
目前基于CO2检测的自动漏气监测设备,能够自动优化气囊压力,选择最小压力。由于气囊上下存在明显的CO2分压差,如果在气囊上能够测到CO2,就认为气囊存在漏气,此时设备会自动补给一定的气囊压,以使其达到最佳。还有RCT研究使用基于声门下测量CO2水平的自动气囊压力控制,结果显示气囊压分布相对稳定,漏气比例也很低,对于预防VAP有很好的效果[16, 17]。
在密闭式吸痰条件下,吸引时间越长,负压越大,医源性误吸发生风险越高。迄今为止也没有证据表明密闭式吸痰比开放式吸痰在预防VAP方面更具优势。一项Meta分析共纳入15项研究,VAP(8项研究1272例患者)和死亡率(4项研究106例患者)方面未发现显著差异,动脉血氧饱和度(5项研究109例患者)、动脉血氧分压(2项研究19例患者)和分泌物去除(2项研究37例患者)尚无结论;与开放式吸痰相比,密闭式吸痰气管内抽吸显著降低了心率的变化和平均动脉压的变化,但增加了定植,而且密闭式吸痰似乎比开放式吸痰费用更高[19]。
# 三、其他 #
研究显示,与不使用PEEP相比,使用PEEP能够降低VAP发生率[21]。不同的PEEP和气道峰压(PIP)不会改变液体泄漏或气道压力下降[22]。因此,PEEP对于预防VAP可能有效。
# 四、小结 #
参考文献
[1] Lucangelo U, Zin WA, Antonaglia V, et al. Effect of positive expiratory pressure and type of tracheal cuff on the incidence of aspiration in mechanically ventilated patients in an intensive care unit[J]. Crit Care Med, 2008, 36(2):409-413.
[2] Vijai M N, Ravi P R, Setlur R, et al. Efficacy of intermittent sub-glottic suctioning in prevention of ventilator-associated pneumonia- A preliminary study of 100 patients[J]. Indian J Anaesth, 2016, 60(5):319-324.
[3] Wen Z, Zhang H, Ding J, et al. Continuous Versus Intermittent Subglottic Secretion Drainage to Prevent Ventilator-Associated Pneumonia: A Systematic Review[J]. Crit Care Nurse, 2017, 37(5):e10-e17.
[4] Li J, Zong Y, Zhou Q, et al. Evaluation of the Safety and Effectiveness of the Rapid Flow Expulsion Maneuver to Clear Subglottic Secretions in Vitro and in Vivo[J]. Respir Care. 2017 Aug;62(8):1007-1013.
[5] Ramírez-Sarmiento A, Aya O, Cáceres-Rivera D, et al. Invention and Pilot Study of the Efficacy and Safety of the SUPRAtube Device in Continuous Supraglottic Aspiration for Intubated and Mechanically Ventilated Patients[J]. Med Devices (Auckl), 2021, 14:287-297.
[6] Tokmaji G, Vermeulen H, Müller M C, et al. Silver-coated endotracheal tubes for prevention of ventilator-associated pneumonia in critically ill patients[J]. Cochrane Database Syst Rev, 2015, 2015(8):CD009201.
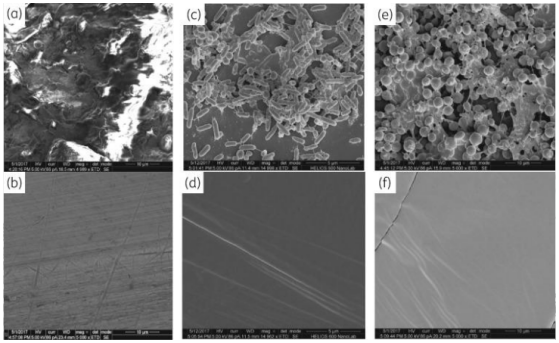
[7] Mann E E, Magin C M, Mettetal M R, et al. Micropatterned Endotracheal Tubes Reduce Secretion-Related Lumen Occlusion. Ann Biomed Eng, 2016, 44(12):3645-3654.
[8] Monsel A, Lu Q, Le Corre M, et al. Tapered-cuff Endotracheal Tube Does Not Prevent Early Postoperative Pneumonia Compared with Spherical-cuff Endotracheal Tube after Major Vascular Surgery: A Randomized Controlled Trial[J]. Anesthesiology, 2016, 124(5):1041-1052.
[9] Miller M A, Arndt J L, Konkle M A, et al. A polyurethane cuffed endotracheal tube is associated with decreased rates of ventilator-associated pneumonia[J]. J Crit Care, 2011, 26(3):280-286.
[10] Mariyaselvam M Z, Marsh L L, Bamford S, et al. Endotracheal tubes and fluid aspiration: an in vitro evaluation of new cuff technologies[J]. BMC Anesthesiol, 2017, 17(1):36.
[11] Harm F, Zuercher M, Bassi M, et al. Prospective observational study on tracheal tube cuff pressures in emergency patients--is neglecting the problem the problem?[J]. Scand J Trauma Resusc Emerg Med, 2013, 21:83.
[12] Lorente L, Lecuona M, Jiménez A, et al. Continuous endotracheal tube cuff pressure control system protects against ventilator-associated pneumonia[J]. Crit Care, 2014, 18(2):R77.
[13] Sevdi M S, Demirgan S, Erkalp K, et al. Continuous Endotracheal Tube Cuff Pressure Control Decreases Incidence of Ventilator-Associated Pneumonia in Patients with Traumatic Brain Injury[J]. J Invest Surg, 2022, 35(3):525-530.
[14] Lorente L, Lecuona M, Jiménez A, et al. Influence of an endotracheal tube with polyurethane cuff and subglottic secretion drainage on pneumonia[J]. Am J Respir Crit Care Med, 2007, 176(11):1079-1083.
[15] Lorente L, Lecuona M, Jiménez A, et al. Subglottic secretion drainage and continuous control of cuff pressure used together save health care costs[J]. Am J Infect Control, 2014, 42(10):1101-1105.
[16] Efrati S, Bolotin G, Levi L, et al. Optimization of Endotracheal Tube Cuff Pressure by Monitoring CO2 Levels in the Subglottic Space in Mechanically Ventilated Patients: A Randomized Controlled Trial[J]. Anesth Analg, 2017, 125(4):1309-1315.
[17] De Pascale G, Pennisi M A, Vallecoccia M S, et al. CO2 driven endotracheal tube cuff control in critically ill patients: A randomized controlled study[J]. PLoS One, 2017, 12(5):e0175476.
[18] Coppadoro A, Bellani G, Bronco A, et al. The use of a novel cleaning closed suction system reduces the volume of secretions within the endotracheal tube as assessed by micro-computed tomography: a randomized clinical trial[J]. Ann Intensive Care, 2015, 5(1):57.
[19] Jongerden I P, Rovers M M, Grypdonck M H, et al. Open and closed endotracheal suction systems in mechanically ventilated intensive care patients: a meta-analysis[J]. Crit Care Med, 2007, 35(1):260-270.
[20] Staudinger T, Bojic A, Holzinger U, et al. Continuous lateral rotation therapy to prevent ventilator-associated pneumonia[J]. Crit Care Med, 2010, 38(2):486-490.
[21] Manzano F, Fernández-Mondéjar E, Colmenero M, et al. Positive-end expiratory pressure reduces incidence of ventilator-associated pneumonia in nonhypoxemic patients[J]. Crit Care Med, 2008, 36(8):2225-2231.
[22] Dave M H, Frotzler A, Weiss M. Closed tracheal suction and fluid aspiration past the tracheal tube. Impact of tube cuff and airway pressure[J]. Minerva Anestesiol, 2011, 77(2):166-171.
[23] Weng H, Li JG, Mao Z, et al. Probiotics for Preventing Ventilator-Associated Pneumonia in Mechanically Ventilated Patients: A Meta- Analysis with Trial Sequential Analysis[J]. Front Pharmacol, 2017, 8:717.
[24] Marcus EL, Yosef H, Borkow G, et al. Reduction of health care-associated infection indicators by copper oxide-impregnated textiles: Crossover, double-blind controlled study in chronic ventilator-dependent patients[J]. Am J Infect Control, 2017, 45(4):401-403.
作者简介
河北医科大学第二医院呼吸与危重症医学一科 副主任医师
河北省医师协会呼吸医师分会秘书
THORAX杂志青年编委
参编著作3部,发表SCI 2篇
获得发明专利1项
参与国家级及省部级课题多项
主要研究方向:急性呼吸窘迫综合征
 后可发表评论
后可发表评论



友情链接
联系我们
 公众号
公众号
 客服微信
客服微信