登录方式
方式一:
PC端网页:www.rccrc.cn
输入账号密码登录,可将此网址收藏并保存密码方便下次登录
方式二:
手机端网页:www.rccrc.cn
输入账号密码登录,可将此网址添加至手机桌面并保存密码方便下次登录
方式三:
【重症肺言】微信公众号
输入账号密码登录
注:账号具有唯一性,即同一个账号不能在两个地方同时登录。
作者:夏金根
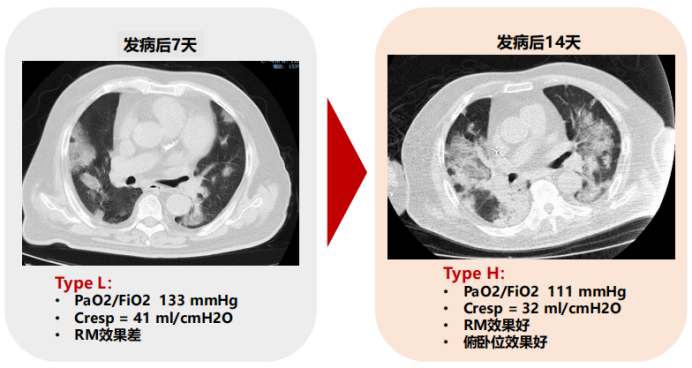
COVID-19 ARDS病理生理机制与自然病程
图源:Anesthesiology, 2021, 134(2):270-282.
图源:Eur Respir J, 2020, 56(3):2002049.


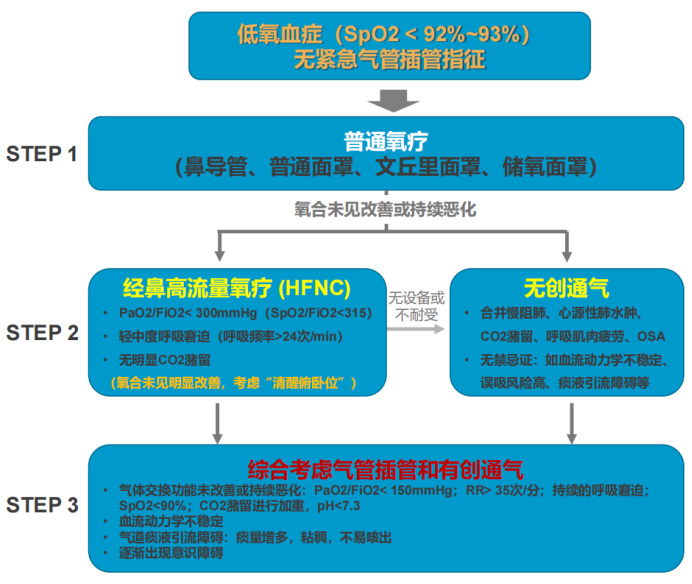
无创呼吸支持方式主要包括经鼻高流量氧疗(HFNO)和无创正压通气(NPPV)。在国外,无创正压通气又分为持续气道正压通气(CPAP)和压力支持通气(PSV),它们各自有不同的连接方式,包括口鼻面罩和头盔。
(1)HFNO:是近年来临床应用非常广泛一种呼吸支持方式,其结构比较简单,患者舒适度较好,操作简便,主要涉及三个参数:气体的温度、流量和氧气浓度。其所产生的生理学效应包括:①稳定吸入气体的浓度;②产生呼气末正压(PEEP)样效应(2~7 cmH2O),增大流量、闭口呼吸可增加呼气末压力;③增加通气效率:减少上呼吸道的死腔量;④改善呼吸形式;⑤改善气道的温湿化功能:增加患者的舒适性和耐受性,改善分泌物的引流和排除。
(2)NPPV:NPPV的支持水平更高,并且压力恒定,而HFNO是流量恒定;NPPV患者耐受性差,并且死腔量增加,其优势是有吸气辅助。理论上来讲,在改善呼吸衰竭(Ⅰ型和Ⅱ型)方面,NPPV应该比HFNO更好,但一些研究结果显示,NPPV的效果并不优于HFNO。对于低氧性呼吸衰竭、无二氧化碳潴留、呼吸频率增快的患者,HFNO有一定优势,能够降低患者气管插管率;此外,ICU病死率和90 d病死率均有明显下降[9]。
为什么NPPV治疗低氧性呼吸衰竭失败率高?对于NPPV治疗低氧性呼吸衰竭,因缺乏足够的证据,加之各项研究之间的异质性很大,在近年的指南中并没有推荐。查阅相关文献发现,NPPV治疗低氧性呼吸衰竭的气管插管率(30%~85%)和病死率(15%~71%)的波动范围非常大,其中也有很多原因,包括:①研究中病种的不均一性;②病情危重、复杂,患者恢复慢;③需要高的PEEP和吸气压力;④NPPV不耐受和人机对抗明显:漏气、呼吸频率快、MV大;⑤NPPV可能加重肺损伤:呼吸驱动增强,潮气量增大,分钟通气量过高,都会导致肺损伤加重;⑥NPPV可能掩盖病情进展,延误治疗时机;⑦对该技术水平和床旁管理的要求较高。
对于非COVID-19患者,ESR临床实践指南仍然推荐HFNO,急性低氧性呼吸衰竭患者对这种呼吸支持方式的获益可能更大[10]。对于COVID-19患者,NPPV的效果如何?2022年发表了很多高质量的RCT研究,但相关的Meta分析较少,各项研究得出的结论不同,有研究发现HFNO更好,也有研究发现NPPV更好,所以目前没有非常明确的证据提示临床更应该选用哪种呼吸支持方式。在WHO指南及美国NIH指南中,虽然证据级别不是特别高,但与普通氧疗相比,仍然推荐使用HFNO或NPPV。
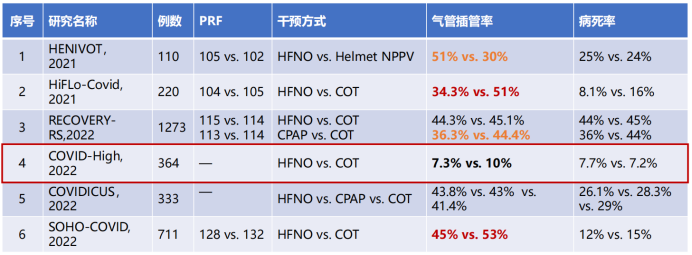
2022发表的样本量较大的文献显示[11-16],与普通氧疗相比,HFNO的确具有优势,虽然二者病死率之间无显著差异,但气管插管率下降,这在很大程度上减轻了医疗负担以及患者对呼吸机通气的需求。在NPPV支持方式中,头盔这种方式是好的,但国内目前没有这种方式,需要更多证据来证实何种通气策略更好。下图第4项研究中的气管插管率较低,因为纳入患者的病情严重程度较低。因此,对于轻症患者,HFNO和普通氧疗之间并没有明显差异。对于普通的轻度低氧血症患者,普通氧疗即可。




参考文献
[1] Tzotzos S J, Fischer B, Fischer H, et al. Incidence of ARDS and outcomes in hospitalized patients with COVID-19: a global literature survey[J]. Crit Care, 2020, 24(1):516.
[2] Williams G W, Berg N K, Reskallah A, et al. Acute Respiratory Distress Syndrome[J]. Anesthesiology, 2021, 134(2):270-282.
[3] Acosta M A T, Singer B D. Pathogenesis of COVID-19-induced ARDS: implications for an ageing population[J]. Eur Respir J, 2020, 56(3):2002049.
[4] Habashi N M, Camporota L, Gatto L A, et al. Functional pathophysiology of SARS-CoV-2-induced acute lung injury and clinical implications[J]. J Appl Physiol (1985), 2021, 130(3):877-891.
[5] Gattinoni L, Coppola S, Cressoni M, et al. COVID-19 Does Not Lead to a "Typical" Acute Respiratory Distress Syndrome[J]. Am J Respir Crit Care Med, 2020, 201(10):1299-1300.
[6] Gattinoni L, Chiumello D, Caironi P, et al. COVID-19 pneumonia: different respiratory treatments for different phenotypes?[J]. Intensive Care Med, 2020, 46(6):1099-1102.
[7] Helmerhorst H J F, Arts D L, Schultz M J, et al. Metrics of Arterial Hyperoxia and Associated Outcomes in Critical Care[J]. Crit Care Med, 2017, 45(2):187-195.
[8] Siemieniuk R A C, Chu D K, Kim L H, et al. Oxygen therapy for acutely ill medical patients: a clinical practice guideline[J]. BMJ, 2018 Oct 24;363:k4169. doi: 10.1136/bmj.k4169.
[9] Frat J P, Thille A W, Mercat A, et al. High-flow oxygen through nasal cannula in acute hypoxemic respiratory failure[J]. N Engl J Med, 2015, 372(23):2185-2196.
[10] Oczkowski S, BErgan B, Bos L, et al. ERS clinical practice guidelines: high-flow nasal cannula in acute respiratory failure[J]. Eur Respir J, 2022, 59(4):2101574.
[11] Grieco D L, Menga L S, Cesarano M, et al. Effect of Helmet Noninvasive Ventilation vs High-Flow Nasal Oxygen on Days Free of Respiratory Support in Patients With COVID-19 and Moderate to Severe Hypoxemic Respiratory Failure: The HENIVOT Randomized Clinical Trial[J]. JAMA, 2021, 325(17):1731-1743.
[12] Ospina-Tascón G A, Calderón-Tapia L E, García A F, et al. Effect of High-Flow Oxygen Therapy vs Conventional Oxygen Therapy on Invasive Mechanical Ventilation and Clinical Recovery in Patients With Severe COVID-19: A Randomized Clinical TrialClinical Trial[J]. JAMA, 2021, 326(21):2161-2171.
[13] Perkins G D, Ji C, Connolly B A, et al. Effect of Noninvasive Respiratory Strategies on Intubation or Mortality Among Patients With Acute Hypoxemic Respiratory Failure and COVID-19: The RECOVERY-RS Randomized Clinical Trial[J]. JAMA, 2022, 327(6):546-558.
[14] Crimi C, Noto A, Madotto F, et al. High-flow nasal oxygen versus conventional oxygen therapy in patients with COVID-19 pneumonia and mild hypoxaemia: a randomised controlled trial[J]. Thorax. 2022, thoraxjnl-2022-218806.
[15] Bouadma L, Mekontso-Dessap A, Burdet C, et al. High-Dose Dexamethasone and Oxygen Support Strategies in Intensive Care Unit Patients With Severe COVID-19 Acute Hypoxemic Respiratory Failure: The COVIDICUS Randomized Clinical Trial[J]. JAMA Intern Med, 2022, 182(9):906-916.
[16] Frat J P, Quenot J P, Badie J, et al. Effect of High-Flow Nasal Cannula Oxygen vs Standard Oxygen Therapy on Mortality in Patients With Respiratory Failure Due to COVID-19: The SOHO-COVID Randomized Clinical Trial[J]. JAMA, 2022, 328(12):1212-1222.
[17] Alhazzani W, Møller M H, Arabi Y M, et al. Surviving Sepsis Campaign: guidelines on the management of critically ill adults with Coronavirus Disease 2019 (COVID-19)[J]. Intensive Care Med, 2020, 46:854-887.
[18] COVID-19 Treatment Guidelines Panel. Coronavirus Disease 2019 (COVID-19) Treatment Guidelines. National Institutes of Health[J]. Crit Care Med. 2021 Mar 1;49(3):e219-e234.
[19] Botta M, Tsonas A M, Pillay J, et al. Ventilation management and clinical outcomes in invasively ventilated patients with COVID-19 (PRoVENT-COVID): a national, multicentre, observational cohort study[J]. Lancet Respir Med, 2021, 9(2):139-148.
[20] Goligher E C, Costa E L V, Yarnell V G, et al. Effect of Lowering Vt on Mortality in Acute Respiratory Distress Syndrome Varies with Respiratory System Elastance[J]. Am J Respir Crit Care Med. 2021 Jun 1;203(11):1378-1385.
[21] McGuinness G, Zhan G, Rosenberg N, et al. Increased Incidence of Barotrauma in Patients with COVID-19 on Invasive Mechanical Ventilation[J]. Radiology, 2020, 297(2):E252-E262.
[22] Shrestha D B, Sedhai Y R, Budhathoki P, et al. Pulmonary barotrauma in COVID-19: A systematic review and meta-analysis[J]. Ann Med Surg (Lond), 2022, 73:103221.
[23] Grasselli G, Scaravilli V, Mangioni D, et al. Hospital-Acquired Infections in Critically Ill Patients With COVID-19[J]. Chest. 2021 Aug;160(2):454-465.
[24] Maes M, Higginson E, Pereira-Dias J, et al. Ventilator-associated pneumonia in critically ill patients with COVID-19[J]. Crit Care, 2021, 25(1):25.
[25] Wicky P H, Niedermann M S, Timsit T F. Ventilator-associated pneumonia in the era of COVID-19 pandemic: How common and what is the impact?[J]. Crit Care, 2021, 25(1):153.
作者简介
中日友好医院呼吸中心呼吸与危重症医学科副主任呼吸治疗师
中华医学会呼吸病学分会呼吸治疗学学组委员
中国医师协会呼吸医师分会呼吸相关职业发展工作委员会委员
中国医学装备协会呼吸病学装备专业委员会第一届委员
中国病理生理学会危重病专业委员会第一届呼吸治疗学组委员
中国康复医学会呼吸康复委员会委员
中国医学救援协会重症医学分会理事会理
*本文根据“Omicron变异株所致重症Covid-19临床救治实战系列”第五期视频整理,感谢夏金根呼吸治疗师予以审核。
 后可发表评论
后可发表评论

相关推荐
1
詹庆元教授|关于制作「重症COVID-19临床救治专家推荐意见临床实施简表」的推荐及说明
7465
2
翟振国教授|重症新冠患者的抗凝治疗:如何平衡血栓和出血的风险
6756
3
COVID-19炎症因子及免疫失衡指标&共感染
4228
4
重症COVID-19病例分享-2
3968
5
重症新冠合并感染的临床流行病学
3680
6
新冠病毒肺部感染影像学特征及动态演变
3556
7
我国Omicron变异株所致重症COVID-19的流行病学
3422
8
重症新冠肺炎的临床表现
3394
9
詹庆元教授:重症新冠感染救治的几个关键问题
3208
10
重症COVID-19病例分享-7
3187


友情链接
联系我们
 公众号
公众号
 客服微信
客服微信